Mehr Fokus im Alltag: Entdecken Sie die Kraft des Magnetarmbands zur Konzentration!
Magnetarmbänder sind nicht nur schmückende Accessoires, sondern können auch einen erheblichen Einfluss auf unsere Konzentration und Fokussierung haben. In diesem ...
Die Zukunft des Schachs: Innovationen und Trends
Wenn du ein begeisterter Schachspieler bist, wird dich dieses Thema wahrscheinlich interessieren. Die digitalen Innovationen und Trends beeinflussen bereits stark ...
Schach in Kunst und Kultur: Einflüsse und Darstellungen
Hast du dich jemals gefragt, warum das Schachspiel so oft in Filmen, Büchern oder Liedern auftaucht? Oder warum weltberühmte Maler ...
Faszination Schachvarianten: Von Blitz bis Fischer Random
Hallo und willkommen zu dieser Reise durch die faszinierende Welt der Schachvarianten. Du kennst Schach vielleicht als zeitloses Spiel der ...
Frauen im Schach: Geschichte, Herausforderungen und Erfolge
Einst galt Schach als ein Spiel für Männer - ein Schlachtfeld, auf dem nur die Stärksten überleben. Im Laufe der ...
Porträts der Schachgroßmeister: Legenden des Spiels
Willkommen zur faszinierenden Welt des Schachs! In 'Porträts der Schachgroßmeister: Legenden des Spiels' öffnen wir das faszinierende Buch der Schachgeschichte ...
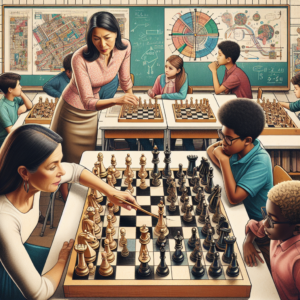
Schach im Bildungsbereich: Lernen durch Logik
Lieber Schachfreund, hast du dich schon einmal gefragt, warum Schach oft als "Das Spiel der Könige" bezeichnet wird? Das liegt ...
Schach und Künstliche Intelligenz: Die Ära der Supercomputer
Schon immer war das Spiel Schach ein Symbole für Intelligenz und taktisches Geschick. Doch in der Ära der Künstlichen Intelligenz ...
Psychologie im Schach: Mentale Strategien der Meister
Wenn du das fesselnde und komplexe Spiel Schach spielst, solltest du wissen, dass es um weit mehr als nur um ...
Grundlagen der Schachstrategie: Eröffnungen und Taktiken
Willkommen zu deinem umfassenden Leitfaden zu den Grundlagen der Schachstrategie, in dem sich alles um Eröffnungen und Taktiken dreht. Wenn ...
Die Geschichte des Schachs: Eine Zeitreise
Willkommen zur Zeitreise in die faszinierende Welt des Schachs! Wenn du schon immer wissen wolltest, wie dieses strategische Brettspiel entstanden ...